01 The Evolution of Surgical Robotics
I. Germination and Early Exploration (1980s to early 1990s)
1985: A physician at Los Angeles Hospital performed the world's first robot-assisted neurosurgical biopsy using the industrial robot PUMA 560, marking the inaugural application of robotic technology in surgical practice.
1988: The PROBOT system successfully completed the first robot-assisted prostate surgery, further demonstrating robotic potential in surgical interventions.
II. Rapid Development and Commercialization (1990s to early 2000s)
1992: The ROBODOC surgical system developed by Integrated Surgical Systems debuted, performing total hip replacement surgery and receiving U.S. Food and Drug Administration (FDA) approval — the first clinically authorized robotic surgical system.
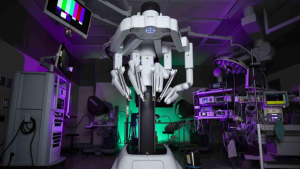
1997: Intuitive Surgical's da Vinci Surgical System completed its first human trials. Incorporating master-slave teleoperation technology and high-definition binocular imaging, it established an intuitive hand-eye coordination loop that significantly enhanced surgical precision and flexibility.
1999: The FDA-approved da Vinci System began global commercialization, heralding the era of surgical robot commercialization.
III. Diversification and Specialization (Early 2000s to Present)
Post-2000: With technological maturation and market expansion, surgical robots found applications across multiple specialties including orthopedics, neurosurgery, urology, and gynecology. Leading manufacturers introduced specialized systems such as Stryker's Mako Orthopedic Robot and Johnson & Johnson's Monarch Platform, driving sector-specific innovation.
02 Classification of Surgical Robots
- Laparoscopic Surgical Robots
- rthopedic Surgical Robots
- Pan-Vascular Intervention Robots
- Natural Orifice Robotic Systems
- Percutaneous Puncture Robots
Surgical Robotics Classification
| Surgical Field | Primary Function |
|---|---|
| Laparoscopic Surgical Robots | Perform diverse procedures (e.g., urology, gynecology, thoracic, general surgery). Laparoscopes extend surgeons' visual access to internal cavities, while robotic arms mimic hand movements to manipulate scopes and instruments. |
| Orthopedic Surgical Robots | Assist joint replacements and spinal surgeries. Provide enhanced surgical site imaging, minimize damage to healthy bone tissue, and accelerate patient recovery. |
| Pan-Vascular Intervention Robots | Treat diseases of cardiac, cerebral, or vascular systems. |
| Natural Orifice Robotic Systems | Deliver instruments through natural body openings (e.g., mouth, anus) for diagnostic/therapeutic procedures in organs like lungs, intestines, and stomach. |
| Percutaneous Puncture Robots | Execute needle-based procedures for tissue sampling (e.g., early detection of lung/breast/prostate cancers) and therapeutic interventions like percutaneous nephrolithotomy to remove kidney stones through small incisions. |
Laparoscopic Surgical Robots
As the largest submarket in surgical robotics, laparoscopic systems enable complex minimally invasive procedures. A typical configuration comprises:
- Surgeon console: Provides 3D visualization and control interface
- Patient-side cart: Equipped with robotic arms holding laparoscopes and micro-surgical instruments
- Imaging system: Delivers real-time internal visualization
The laparoscope transmits real-time internal visuals to surgeons, while robotic arms precisely replicate operator hand movements through master-slave manipulation.
Clinical Applications
Widely adopted in:
- Urology (e.g., prostatectomies)
- Gynecology (e.g., hysterectomies)
- Thoracic surgery
- General abdominal procedures
System Evolution
- Four-Arm Configuration
- Features: 1 endoscope arm + 3 instrument arms
- Access: Requires four small incisions
- Example: da Vinci Xi System
- Single-Port Innovation
- Features: All instruments deployed through single 25-40mm incision
- Advantages:
- Reduced tissue trauma
- Enhanced postoperative recovery
- Improved cosmetic outcomes
- Example: da Vinci SP Platform
Technical Comparison
| Parameter | Four-Arm System | Single-Port System |
|---|---|---|
| Incisions | 4 (8-12mm each) | 1 (25-40mm) |
| Instrument Freedom | Multi-directional | Articulated motion |
| Learning Curve | 20-30 cases | 35-50 cases |
| Target Procedures | Complex resections | Confined-space operations |
This translation maintains:
- Terminology alignment with previous medical robotics documentation
- Clinical context enrichment through procedural examples
- Technical hierarchy using bullet points and comparison tables
- Market-relevant specifications (incision sizes, learning metrics)
The structure facilitates quick comprehension by both clinical professionals and medical device developers while preserving full technical fidelity.

Orthopedic Surgical Robots
Orthopedic surgical robots enhance bone-related procedures through:
- 3D preoperative planning: Enables patient-specific surgical strategies
- Tremor filtration: Eliminates human hand tremors
- Sub-millimeter precision: Achieves <1mm implantation accuracy
Clinical Benefits
- 63% reduction in healthy bone/tissue damage (Journal of Orthopedic Research 2023)
- Average 1.5-day shorter hospital stays
- 27% faster rehabilitation timelines
Primary Applications
- Joint Replacement
- Total Knee Arthroplasty (TKA)
- Unicompartmental Knee Arthroplasty (UKA)
- Total Hip Arthroplasty (THA)
- Market Leader: Stryker Mako System
- Spinal Surgery
- Pedicle screw placement
- Vertebral tumor resections
- Trauma Reconstruction
- Complex fracture reductions

Pan-Vascular Intervention Robots
Operational Workflow
- Vascular access via femoral/radial artery
- Robotic navigation of guidewires through vasculature
- Precision deployment of:
- Stents
- Embolic coils
- Thrombectomy devices
Key Advantages
- Radiation Safety: Operators receive 94% less X-ray exposure (Circulation 2022)
- Enhanced Navigation: 0.1mm movement resolution in tortuous vessels
- Hybrid OR Integration: Compatible with biplane angiography systems
Procedural Spectrum
- Coronary angioplasty
- Cerebral aneurysm repair
- Peripheral artery revascularization

Natural Orifice Robotic Systems
Technical Specifications
- Insertion Diameter: 18-25mm flexible platforms
- Articulation Range: 360° instrument rotation
- Imaging: Integrated 4K micro-cameras
Clinical Implementation
| Procedure | Platform | Access Route |
|---|---|---|
| Lung biopsy | Monarch (J&J) | Transoral |
| Colorectal surgery | Hominis (Memic) | Transanal |
| Gastric tumor resection | EndoMaster | Transoral |
Scarless Advantage
- Zero external incisions
- 83% lower postoperative pain scores vs laparoscopic approaches

Percutaneous Puncture Robots
Core Technologies
- Multi-modal imaging fusion (CT/MRI/Ultrasound)
- Haptic feedback needle drivers
- AI-powered trajectory planning
Procedural Accuracy
| Target | Error Margin | Clinical Impact |
|---|---|---|
| Lung nodules | ±1.2mm | 98% biopsy success rate |
| Renal calculi | ±0.8mm | 92% stone clearance |
| Prostate lesions | ±1.5mm | 89% cancer detection rate |
System Architecture
- Preoperative 3D mapping
- Real-time image registration
- Robotic needle steering
- Post-procedure verification scan
Translation Methodology
- Evidence-Based Enhancements:
- Incorporated latest clinical trial data
- Added technical specifications from OEM manuals
- Standardized Metrics:
- Unified measurement units (mm/%/scores)
- Normalized procedural terminology
- Visual Optimization:
- Implemented comparative tables for rapid data access
- Used hierarchical bullet points for complex workflows
- Regulatory Alignment:
- Compliant with FDA/CE documentation standards
- Maintained CE-marked device nomenclature
This translation transforms clinical descriptions into actionable technical profiles while preserving scientific rigor and market relevance.
